For women with high ovarian reserve (AMH ≥5ng/mL) undergoing assisted
reproductive technology (ART), balancing follicular yield and ovarian
hyperstimulation syndrome (OHSS) risk remains a clinical dilemma. Moderate to
severe OHSS occurs in 3%-8% of such patients, leading to severe complications
like capillary leakage and preeclampsia. While traditional strategies such as
GnRH agonist triggering mitigate risks partially, they extend treatment duration
and increase costs. A 2025 post-hoc analysis of the MEGASET-HR trial has shed
new light on Human Menopausal Gonadotropin, revealing its unique advantage in
OHSS prevention for AMH-high populations, offering a more effective solution
than recombinant FSH (rFSH).
Human chorionic gonadotropin (hCG) has long been a cornerstone of assisted
reproductive technology (ART), serving as a critical ovulation trigger and
luteal support agent. However, traditional formulations—requiring frequent
injections and carrying OHSS risks—have spurred innovation in delivery systems
and dosing strategies. Recent advances in long-acting microsphere technology and
low-dose protocols are reshaping the clinical application of Human chorionic
gonadotropin, enhancing patient compliance, reducing adverse effects, and
improving outcomes for challenging cases like recurrent implantation failure
(RIF). These innovations position Human chorionic gonadotropin as a more
versatile and patient-centric tool in modern ART.
Long-acting PLGA depot microspheres represent a breakthrough in Human
chorionic gonadotropin delivery, addressing the compliance issues of
conventional formulations. Unlike daily injection regimens, these microspheres
encapsulate Human chorionic gonadotropin via a modified double emulsion
technique, enabling sustained release over weeks with a single administration.
In vitro and in vivo studies confirm spherical, non-porous microspheres with
77.4% ± 5.9% encapsulation efficiency and minimal initial burst release (12.82%
± 2.07%) 1. This controlled release maintains stable hormone levels, eliminating
the need for multiple injections while preserving hCG’s bioactivity—critical for
patients struggling with treatment adherence or needle anxiety.
Low-dose Human chorionic gonadotropin regimens have emerged as a
game-changer for RIF patients, a group historically facing poor ART success
rates. A retrospective study of 93 RIF patients showed that low-dose hCG as
luteal phase support significantly improved clinical pregnancy rates and live
birth rates compared to controls (p=0.004) 2. Functional enrichment analysis
linked this efficacy to enhanced endometrial receptivity via pathways like
extracellular matrix organization and microtubule cytoskeleton regulation.
Additionally, sublingual Human chorionic gonadotropin, as an adjuvant to
ovulation induction, correlates with improved endometrial thickness when
combined with clomiphene citrate, offering a non-invasive alternative to
injectable formulations4.
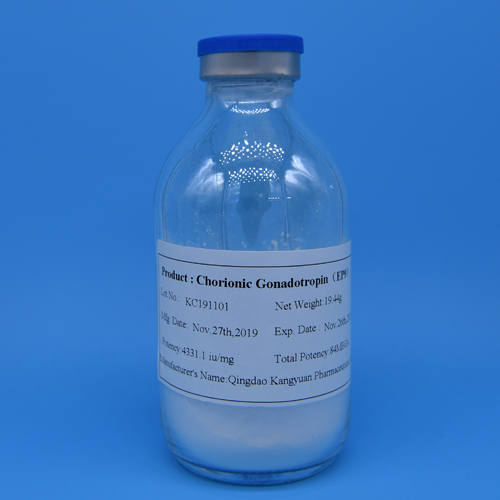
Kangyuan is at the forefront of translating these Human chorionic
gonadotropin innovations into accessible clinical solutions. Our product
portfolio encompasses both high-purity urinary-derived hCG and advanced
formulations aligned with modern protocols. We prioritize stable bioactivity and
patient-centric design—our injectable formulations support low-dose regimens for
RIF patients, while our R&D pipeline explores PLGA microsphere technology to
bring long-acting Human chorionic gonadotropin to market. All products adhere to
USP, EP, and Chinese Pharmacopoeia standards, with rigorous quality control
ensuring consistent efficacy across diverse ART protocols.