For women with high ovarian reserve (AMH ≥5ng/mL) undergoing assisted
reproductive technology (ART), balancing follicular yield and ovarian
hyperstimulation syndrome (OHSS) risk remains a clinical dilemma. Moderate to
severe OHSS occurs in 3%-8% of such patients, leading to severe complications
like capillary leakage and preeclampsia. While traditional strategies such as
GnRH agonist triggering mitigate risks partially, they extend treatment duration
and increase costs. A 2025 post-hoc analysis of the MEGASET-HR trial has shed
new light on Human Menopausal Gonadotropin, revealing its unique advantage in
OHSS prevention for AMH-high populations, offering a more effective solution
than recombinant FSH (rFSH).
Human Menopausal Gonadotropin, particularly in its highly purified (HP-hMG)
form, demonstrates significant OHSS risk reduction independent of oocyte count.
The multi-center trial involving 620 AMH-high patients (21-35 years old) showed
that the total OHSS incidence in the Human Menopausal Gonadotropin group was
only 9.7%, drastically lower than 21.4% in the rFSH group. The advantage was
more pronounced in early OHSS (trigger post ≤9 days), with 6.1% in the HP-hMG
group versus 17.5% in the rFSH group. Even in the extreme scenario of >25
oocytes retrieved, Human Menopausal Gonadotropin maintained an early OHSS rate
of 8.3%, compared to 32.4% in the rFSH group, confirming its independent
protective effect.
The unique pharmacological profile of Human Menopausal Gonadotropin
underlies its safety advantage. Unlike rFSH, which triggers stronger ovarian
responses in high-AMH patients (AMH every 1.54ng/mL increase leads to 1 more
oocyte in rFSH group), Human Menopausal Gonadotropin’s balanced FSH and LH
components regulate follicular development more gently. Notably, GnRH agonist
triggering—once considered a first-line OHSS prevention measure—failed to
eliminate risks, with no significant difference in total OHSS rates between GnRH
agonist and hCG triggering groups. This highlights that choosing Human
Menopausal Gonadotropin is more critical for OHSS control than trigger type.
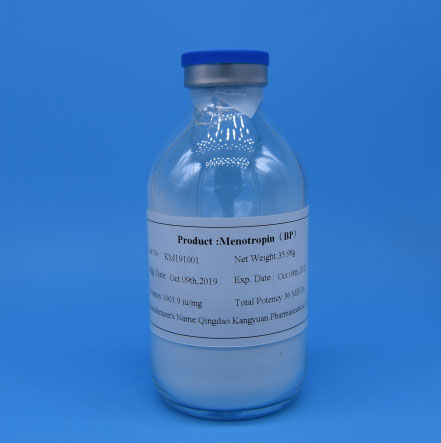
Kangyuan’s Human Menopausal Gonadotropin products are engineered to
maximize this clinical advantage, adhering to strict global quality standards
(USP, EP, Chinese Pharmacopoeia) for high purity and consistent bioactivity. Our
HP-hMG undergoes advanced purification processes to ensure optimal FSH-LH ratio,
replicating physiological hormone secretion to stabilize follicular development.
We offer flexible dosages (75IU, 150IU vials) tailored to individual patient
characteristics—such as age, BMI, and baseline estradiol levels, which the trial
identified as key OHSS predictors. This personalized approach further enhances
safety while maintaining satisfactory pregnancy rates.
As ART shifts toward risk-adapted protocols, Human Menopausal Gonadotropin
emerges as a cornerstone for AMH-high patients, reconciling efficacy and safety.
Kangyuan remains committed to translating cutting-edge clinical evidence into
accessible solutions, providing high-quality Human Menopausal Gonadotropin that
supports clinicians in optimizing OHSS prevention strategies. Our professional
team offers tailored guidance on protocol design, helping integrate HP-hMG into
GnRH antagonist regimens for optimal outcomes. Whether you are a clinic seeking
safer ART solutions for high-response patients or a distributor expanding
reproductive health portfolios, Kangyuan is your trusted partner. Contact us
today to unlock the full potential of Human Menopausal Gonadotropin in your
practice.