In the realm of assisted reproductive technology (ART), advanced-age
patients with diminished ovarian reserve (DOR) pose a significant clinical
challenge, characterized by poor ovarian response and low pregnancy rates. As a
classic gonadotropin preparation containing both follicle-stimulating hormone
(FSH) and luteinizing hormone (LH), Human Menopausal Gonadotropin has long been
utilized in ovulation induction therapy. Recent clinical research has shed new
light on its application value—optimizing the timing of Human Menopausal
Gonadotropin supplementation can significantly improve pregnancy outcomes in
this vulnerable population, offering new hope for infertile couples.
The unique dual-hormone composition of Human Menopausal Gonadotropin
underpins its irreplaceable role in treating DOR patients. Unlike
single-component FSH preparations, it simultaneously supplements FSH to promote
follicular development and LH to enhance follicular maturation, which aligns
with the physiological hormone secretion rhythm of the human body. For
advanced-age DOR patients, whose ovarian sensitivity to gonadotropins declines,
the synergistic effect of FSH and LH in Human Menopausal Gonadotropin can
effectively improve ovarian response, increasing the number of mature oocytes
and available embryos. A multi-center clinical study involving 682 advanced-age
DOR patients confirmed that rational supplementation of Human Menopausal
Gonadotropin could significantly optimize treatment outcomes, especially when
administered at the appropriate stage of follicular development.
The timing of Human Menopausal Gonadotropin supplementation emerges as a
critical factor affecting clinical efficacy. In the GnRH antagonist protocol, a
widely used ART regimen, researchers found that supplementing Human Menopausal
Gonadotropin in the middle and late follicular phase (when the dominant follicle
diameter reaches 10-14 mm) yielded superior results compared to early
supplementation or no supplementation. Specifically, this timing strategy
increased the number of mature oocytes and available embryos, and elevated the
clinical pregnancy rate of fresh embryo transfer cycles from 27.7% to 45.1%. In
contrast, early supplementation starting from the initial stage of ovulation
induction did not show similar benefits, highlighting the importance of
personalized timing based on follicular development status.
Safety and tolerability are additional advantages of Human Menopausal
Gonadotropin in clinical application. As a urinary-derived gonadotropin
preparation, it has undergone decades of clinical verification with a
well-established safety profile. When used under strict medical supervision and
dosage control, the risk of ovarian hyperstimulation syndrome (OHSS) is
effectively managed, which is particularly crucial for advanced-age patients
with compromised physical conditions. Compared to some high-cost recombinant
gonadotropins, Human Menopausal Gonadotropin also offers economic benefits,
reducing the financial burden on patients undergoing long-term ART
treatment.
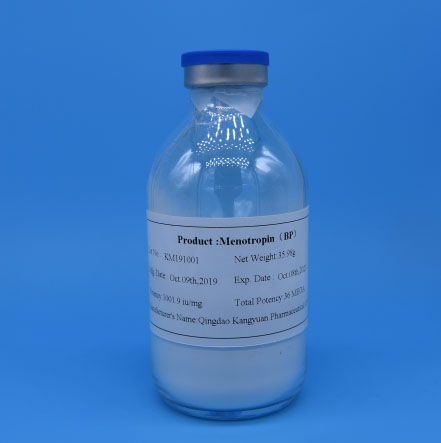
As a professional pharmaceutical manufacturer dedicated to reproductive
health, Kangyuan is committed to providing high-quality Human Menopausal
Gonadotropin products that meet international standards. Our products adhere to
strict quality control systems, from traceable raw material sourcing (urine from
healthy postmenopausal women) to GMP-compliant production processes, ensuring
consistent efficacy and safety. We also collaborate with clinical institutions
to promote the application of evidence-based medicine, helping clinicians
optimize treatment regimens using Human Menopausal Gonadotropin. If you are a
healthcare provider seeking reliable gonadotropin solutions for advanced-age DOR
patients, or an infertile couple exploring ART options, please contact
Kangyuan’s professional team. We will provide tailored product support and
clinical advice to help you navigate the challenges of reproductive treatment
and realize the dream of parenthood.