Refractory ovulatory disorders, such as clomiphene citrate-resistant
polycystic ovarian disease (PCOD), remain a major challenge in fertility
treatment, affecting approximately 15-20% of women seeking assisted
reproduction. For these patients, conventional ovulation induction therapies
often fail to achieve satisfactory follicular development and clinical pregnancy
rates, highlighting the need for more effective and tailored treatment options.
Human Menopausal Gonadotropin (hMG), a combination of follicle-stimulating
hormone (FSH) and luteinizing hormone (LH) derived from the urine of
postmenopausal women, has emerged as a cornerstone in managing refractory cases
due to its unique hormonal balance and proven clinical performance. Unlike
recombinant FSH (rFSH) preparations, hMG’s dual FSH-LH activity closely mimics
physiological ovarian stimulation, making it particularly suitable for patients
with suboptimal response to single-hormone therapies.
The clinical value of Human Menopausal Gonadotropin in refractory ovulatory
disorders is supported by robust real-world evidence. While randomized
controlled trials (RCTs) with small, selected populations have shown
inconsistent results comparing hMG and rFSH, large-scale real-world analyses
have clarified its efficacy in diverse patient groups. A study covering over
28,000 fertility cycles in Germany found that for patients treated with GnRH
agonists (the standard of care in many regions), hMG achieved comparable ongoing
pregnancy and clinical pregnancy rates to rFSH, with no significant differences
in pregnancy loss or ovarian hyperstimulation syndrome (OHSS) incidence. More
importantly, for patients with low LH levels or poor ovarian reserve—common in
refractory cases—Human Menopausal Gonadotropin’s intrinsic LH activity enhances
follicular maturation and improves oocyte quality, addressing a critical unmet
need that single-agent FSH therapies often overlook.
Personalized dosing strategies further amplify the effectiveness of Human
Menopausal Gonadotropin in refractory populations. Due to significant
inter-individual variability in ovarian response to exogenous gonadotropins, a
one-size-fits-all dosage approach often leads to cycle cancellation or
suboptimal outcomes. Clinical guidelines emphasize that hMG dosage should be
adjusted based on real-time monitoring of follicular growth and hormone levels,
such as estrogen and LH concentrations. For clomiphene-resistant PCOD patients,
initiating hMG at a low dose (75-150 IU/day) and gradually titrating upward
reduces OHSS risk while promoting controlled follicular development.
Additionally, combining hMG with GnRH antagonists in personalized protocols has
been shown to improve cycle success rates by suppressing premature
luteinization, a common issue in refractory ovulation induction. These tailored
approaches ensure that Human Menopausal Gonadotropin maximizes therapeutic
benefits while minimizing safety risks.
Cost-effectiveness is another key advantage of Human Menopausal
Gonadotropin in fertility treatment. A systematic review comparing hMG and rFSH
found that despite rFSH achieving a slightly higher mean number of oocytes
retrieved in most studies, the cost per oocyte was comparable for both
therapies. For healthcare systems and patients facing the financial burden of
repeated fertility cycles, hMG offers a clinically effective alternative without
excessive cost. Furthermore, highly purified hMG preparations (such as Menopur)
have improved safety profiles, with reduced antigenicity and fewer
injection-site reactions, enhancing patient adherence to treatment regimens.
Ongoing research continues to refine hMG-based protocols, exploring its
combination with adjuvant therapies to further improve live birth rates in
refractory populations.
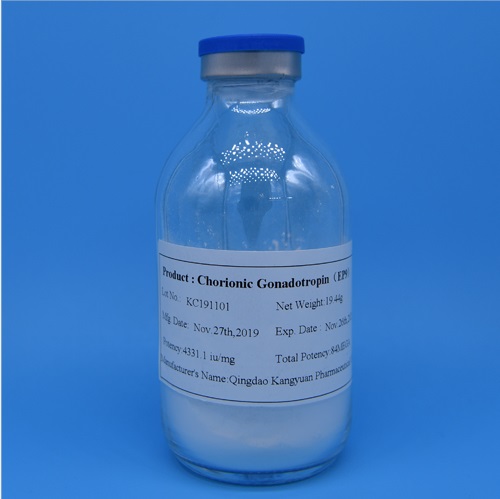
At Kangyuan, we are committed to providing high-quality Human Menopausal
Gonadotropin that meets global regulatory standards, supporting personalized
fertility treatment for patients with refractory ovulatory disorders. Our highly
purified hMG preparations ensure consistent potency and safety, with rigorous
quality control throughout the production process. We collaborate closely with
fertility specialists to offer tailored solutions, including dosage guidance and
protocol optimization, to maximize clinical outcomes. Whether you are a
healthcare provider seeking reliable hMG supplies or a patient exploring
fertility treatment options, our professional team is dedicated to delivering
expert support and personalized care. Contact us today to learn more about how
our Human Menopausal Gonadotropin can support your fertility treatment
journey.